Information for parents and caregivers
The National Guideline for the assessment and diagnosis of autism in Australia sets out 66 Recommendations for how assessments that consider a diagnosis of autism should occur.
The Guideline focuses on the practitioners conducting the assessments, such as doctors and allied health practitioners.
However, parents and caregivers can also use the Guideline to understand the assessment process, including who is involved, and how, where, and when different parts of the assessment are conducted.
Information booklet for parents and caregivers
We have prepared an information booklet that outlines for parents and caregivers what to expect and experience during a clinical assessment and diagnosis of autism, based on the best practice Recommendations in the Guideline. It also provides tips for engaging with practitioners, examples of what good practice should look like, and links to additional information.
Summary information
The following information is a summary of the Guideline and what you can expect for children undergoing an assessment should expect.
The National Guideline for the assessment and diagnosis of autism in Australia sets out 66 Recommendations for how assessments that consider a diagnosis of autism should occur.
The Guideline focuses on the practitioners conducting the assessments, such as doctors and allied health practitioners.
However, parents and caregivers can also use the Guideline to understand the assessment process, including who is involved, and how, where, and when different parts of the assessment are conducted.
What to expect
If your child has been referred for an assessment, you should expect:
 a timely and thorough assessment
a timely and thorough assessment consideration of your unique needs, strengths and resources
consideration of your unique needs, strengths and resources prompt referral to support services based on your functioning and needs (regardless of diagnosis)
prompt referral to support services based on your functioning and needs (regardless of diagnosis) a report summarising the assessment findings and diagnostic decision, explained in person by an expert health professional.
a report summarising the assessment findings and diagnostic decision, explained in person by an expert health professional.
About the Guideline
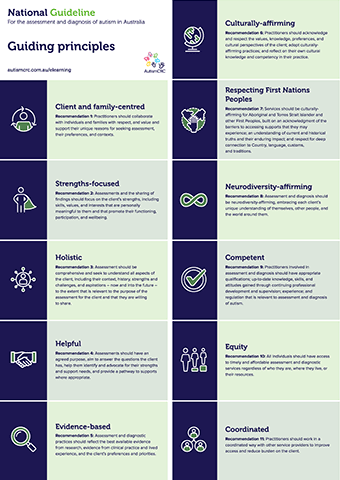
The Guideline helps ensure that practitioners involved in assessment engage in best practice. This means working in ways that are appropriate, evidence-based, and helpful to individuals being assessed and their families.
The Guideline was developed through a rigorous process involving extensive community consultation and evidence review. Notably, members of the autistic and autism communities generously shared their experiences, insights, and views to inform the Guideline.
It is approved by the National Health and Medical Research Council (NHMRC), meaning it meets the highest national standard.
Reasons to get an assessment
The purpose of assessments that consider autism is to better understand your child’s health, development, and wellbeing as the basis for identifying strengths and any support needs.
A proper assessment will not just focus on autism. Instead, it will consider all possible explanations for the aspects of your child’s development that appear to be delayed or different to other children.
Sometimes an assessment will result in a diagnosis of autism, and/or other conditions. The most important thing is that the assessment helps you to understand your child’s strengths and any needs, so that a plan can be put in place to support your child in their ongoing development in ways that effective, safe and desirable to both your child and your family.
Where to begin
As a parent or guardian, you can speak to your child’s health practitioner (e.g., General Practitioner, Aboriginal Health worker) about any questions or concerns about your child’s development. Sometimes, a parent or guardian may be working with a health practitioner for other reasons (e.g., seeking support with learning to talk) and that practitioner may suggest further assessment.
Either way, the health practitioner should listen to and discuss your questions and concerns and take a broad look at your child’s development, health, and wellbeing. First, they may do this themselves or refer to another health practitioner.
If the practitioner thinks your child is showing characteristics of autism, they should then begin to follow the assessment and diagnostic process outlined in the Guideline. It is important to remember, however, that they will not just be thinking about autism. Instead, they will be thinking about all the possible explanations for how your child is developing all the way through the assessment process.
It is important to note that if, at this point, you feel like your questions have not been answered or concerns are not addressed, it is okay to seek a second opinion.
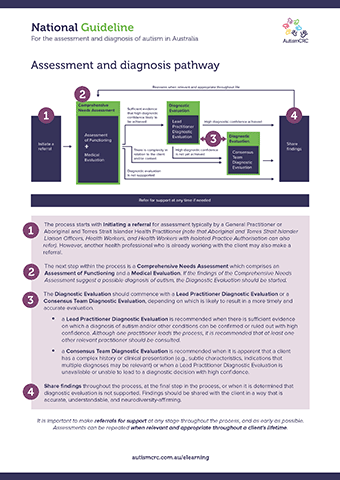
What's involved in an assessment
If further assessment is needed, the next step will be to gain a comprehensive understanding of your child’s health, development, and wellbeing including functional strengths and any support needs.
An Assessment of Functioning involves obtaining a detailed understanding of your child’s abilities and any support needs they might have across a broad range of areas. These areas include cognitive abilities, speech and language function, daily living skills, friendships, and school.
A Medical Evaluation involves a physical examination and other medical tests to understand if there could be medical causes for the behaviours or characteristics that prompted the referral.
Where there are characteristics of autism, a Diagnostic Evaluation is then completed. This may involve the use of additional tools (e.g., parent questionnaires, play-based assessment).
The Guideline explains who should be involved and how the different parts of assessment should happen.
Some aspects of assessment are flexible, for example:
- Sometimes, all parts of the assessment will be conducted separately, while for other children and families, they will happen at once.
- Some children and families will see a small number of practitioners, while others will work with a larger team.
- While all assessments must be in person consultation, sometimes some parts will be conducted by telehealth.
However, there are some aspects of the assessment that are fixed, for example:
- The assessment must include all parts.
- People who lead different aspects of the assessment are recommended to have select qualifications (the Guideline explains this in more detail).
- The assessment must always consider all possible explanations for differences and/or delays in a child’s development (this is called differential diagnosis).
Some possible outcomes
For some children, the assessment leads to a clear finding regarding whether or not autism is an appropriate diagnosis. However, for others, the picture is not so clear, and further assessment may be needed. For example, the team may be expanded to include practitioners with additional expertise, or it may happen over a longer period with more appointments.
It is common for an assessment that considers autism to not result in a diagnosis of autism. For example, a child being very reluctant to engage in social situations may be better explained by anxiety.
At every stage, the practitioners you work with should talk to you about what they are doing, what they are finding, and what they recommend should happen next. They should explain the reasons for their decisions and encourage you to ask questions.
Their job is to listen and help you be fully informed when making decisions. You are always in control of what happens in an assessment that involves your child and family.
After an assessment
After the assessment, the Guideline recommends that the health professionals involved provide you with a written report, explained to you, and, if appropriate, your child in a meeting.
The report will summarise the information collected during the assessment and what this information means. It will also explain any decisions that have been made about a diagnosis and suggest next steps for accessing support services.
Accessing support
Accessing support can, and should, happen at any time it is needed.
Practitioners you work with should ask about what, if any, supports are already in place and if additional supports are needed.
A referral for support should happen as soon as need is identified.
Additional resources
You may wish to download any of the following resources for your reference or display purposes.